As the nation’s daily count of COVID-19 cases continues to rise, we are again seeing a major demand for nurses and travel nurses in facilities across the country. For some of us, we have experienced this public health catastrophe in waves, while others have been working COVID crisis contracts since March. Either way, nurses have demonstrated bravery, compassion, and an unstoppable determination while caring for some of the sickest patients they have seen during their careers.
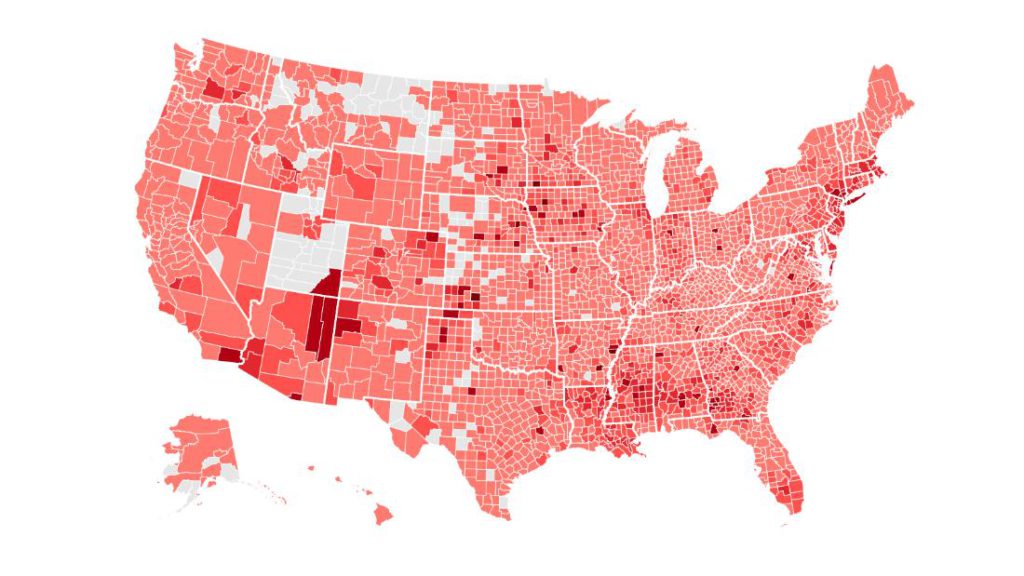 Photo: John Hopkins University
Photo: John Hopkins University
We are also heading into flu season on top of a global health crisis. I am an ICU nurse in Colorado and over the last few weeks I’ve watched our number of coronavirus patients triple. Collectively, nurses are anticipating a busy season coupled with a large amount of high acuity patients. I think it feels a bit different this time; we almost feel like we know what we are up against. This time around, healthcare providers have experience in how the virus behaves and are able to predict how their patients’ conditions might change.
COVID-19 and Travel Nursing
We have hired over 15 travel nurses to supplement our staffing. The hospital is driving up their infection control and assuring we have the PPE available when we need it. My days are once again becoming filled with donning and doffing, trying to hydrate, and helping out my team as we try to manage our patients that seem to be getting sicker by the hour.
One Day as a COVID ICU Nurse
The typical day of a COVID-ICU nurse is stressful and fast-paced. This disease has changed how we prepare for work and provide care. I start my day by putting on regular clothes to drive to work. In the past I would have worn my scrubs in, but now the hospital provides surgical scrubs that are washed after each use to avoid us bringing the virus into our homes.
Two weeks ago I’d be wondering if I would be in the ‘COVID pod’, but now all of the pods except one ‘clean area’ have at least one COVID positive patient, with one area having a cluster of 5-7 patients. I change into scrubs as soon as I arrive and pull my respirator and goggles out of my locker, along with a wipeable pouch that contains pens, scissors, clamps, hydro-colloid Band-Aids for my nose (to protect it from the mask rubbing), and all of the other useful nursing tools.
7AM: My COVID ICU Shift Starts
I walk into the COVID area with my orientee. He is a new graduate nurse, but he is learning fast in this new healthcare environment. We are taking a patient that is on hospice after a long and difficult fight with COVID, and another that is on CPAP and gets short of breath with activity, but is otherwise ok. Unfortunately, this is a typical COVID assignment in the ICU- one patient that’s high risk for intubation and another that is very sick or actively passing.
We take report, taking note of family members that will be coming into be with their loved one while he is passing. They are not allowed in the room, but will be outside the door. We arrange to have a phone on speaker in the room next to the patient so he can listen to loving words and prayers from his family.
Just as we finish report, another nurse asks for help because her patient needs to be intubated. It’s 7:30 AM. My orientee starts morning care and meds with his patients, while I help the other nurse gather equipment and staff for the intubation. The patient is relatively unstable and we are all a bit anxious. The breathing tube is successfully inserted with no major event, and we move on.
COVID ICU Nursing: Stay Flexible and Be Prepared to Keep Moving

I am then told that another patient in the pod needs to be started on ECMO. I am the only cardiac nurse in the immediate area, and it would be easiest for me to take the patient and have the other nurse help my preceptee, rather than shuffling staff from other areas. Thankfully, my orientee is far along enough that he is able to manage his patients mostly on his own.
The provider and I enter the room to start an arterial line on the patient before they are cannulated for ECMO. During this procedure, the patient next door starts crashing and has dangerously low oxygen levels. I run through the bathroom (it connects to the next room) and ask the nurse what she needs. I go back and communicate this to the physician who is sterile and can’t leave the bedside. He orders a paralyzing medication, it’s given, and all is well again. It’s 9:30AM. I have had two sips of water and have been in my respirator for about an hour and a half total.
Expect the Unexpected as a COVID ICU Nurse
We start our ECMO cannulation around noon with the CV surgeon. The plan is for venous-venous (V-V) ECMO to assist the patient’s pulmonary function. The procedure is going as planned, the cannulas are inserted successfully, when suddenly the patient starts to lose their blood pressure and heart rate. I yell for epinephrine and one of the operating room staff starts chest compressions. The physician remains calm and changes the plan to venous-arterial (V-A) ECMO, requiring the insertion of a third cannula.
The room is filled with people, I am hanging fluid boluses and blood products, CPR is being performed, a nurse is pushing life-saving medications and shouting them out to the nurse standing outside the door recording. We are trying to keep the door of the negative pressure room closed to limit exposure, but we have to open it for supplies, meds, and additional equipment.
Nurses, Teamwork, and Coronavirus
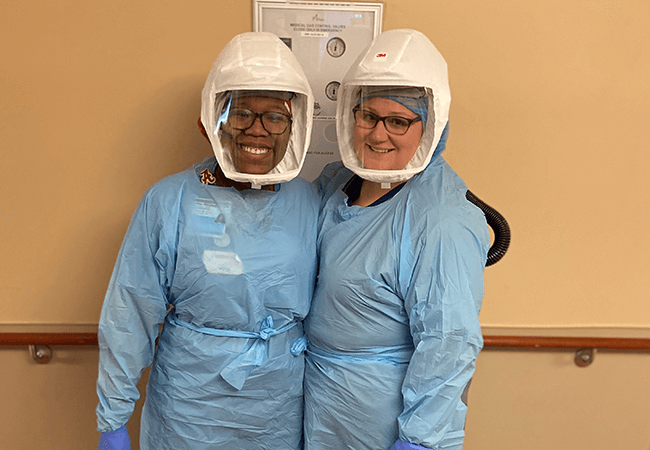
I can’t help but admire my teammates during this chaotic situation. The physicians are communicating calmly, the OR staff is performing their sterile procedure, the nurses are acting as an assembly line for medications and chest compressions, and we all know our role is key in this coordinated dance of providing critical care. Everyone is sweating in their blue plastic gowns, N95s, respirators, and PAPR hoods. Yet, we all are doing everything we can to help each other give the patient the best chance possible.
Thankfully, we had return of circulation and the patient survived. The patient’s family was able to come to the door for five minutes to see them after the arrest. I went out to briefly express my empathy and reassure them I was doing everything in my power to help their loved one.

The patient was successfully put on V-A ECMO and my next few hours were filled with task after task to ensure the patient’s safety. I gave fluids and blood transfusions, drew an exhaustive number of labs, monitored blood sugar every hour and administered insulin, titrated medications that were supporting her blood pressure, and collaborated with a perfusionist to optimize her level of support. I finally exited the room after two and a half hours of being in full PPE. It was 3:00PM. My face hurt and I was very thirsty. My clothes were soaked in sweat and my skin was sticky from the plastic gowns.
PPE and ICU Nursing
My time out of the room was short, but sweet. I had more monitoring to set up, medications to give, charting to complete, and I was still checking in on my orientee (who, thankfully was doing an amazing job!!). I re-entered the room for another few hours, and managed to somehow get out on time, despite the craziness of the shift.

At the end of the day, I think I spent about 10 hours total in my respirator and full PPE. I hate to think this is becoming the norm again. It’s hard to look down the road and face what may be coming. March through May was the most difficult time in my career. Every day was a shift like described above. Emergency after emergency and feeling like despite moving as fast you can, you are constantly behind in care and charting.
Nurse Heroes
I take comfort in knowing I work with an awesome team that always steps up to help one another out. I welcome the travel nurses that have come to help us out during this pandemic and am grateful for their experience and knowledge. All we can do is take it one day at a time and promote awareness and safety in our communities.
Nurses have proven their impact on healthcare this year, and that effect will rollover into 2021. We have helped shape care and how hospitals are staffed in response to the pandemic. Tons of nurses have joined the travel nursing world as opportunities become available to help care for these patients.
Join us while we fight against coronavirus and send aid to those areas most in need.
Thank you to all the nurse and healthcare heroes out there!!!
